This is the last article you can read this month
You can read more article this month
You can read more articles this month
Sorry your limit is up for this month
Reset on:
Please help support the Morning Star by subscribing here
AS health unions, doctors and nurses prepare for strike action over pay offers, a largely ignored, recently released report by the NHS shows the staggering sums being paid out in compensation to those individuals, families and relatives affected by medical negligence due to staff shortages.
The annual report and accounts for NHS Resolution, an arm’s-length body set up to administer claims against GPs and hospital staff, reveals that at the end of the last financial year, the NHS had paid nearly £83 billion in liabilities in relation to historic claims received, or new claims likely to be received in future.
That figure is nearly half of the whole NHS and social care budget for 2021, or enough to build 150 new hospitals.
In the past few years regular reports of failures in NHS trusts maternity, older people, mental health and learning disability services have been exposed.
There has been a 30 per cent increase in clinical claims in the past 10 years of Tory government.
And there were 12,629 claims in the last year, paying out over £2 billion, of which £1 billion went to lawyers and £1.3bn to claimants.
NHS Resolution settled 15,574 clinical and non-clinical claims in 2020/21, 124 more than in 2019/20 when they settled 15,550 claims.
Of these, 11,704 (74.7 per cent) claims were settled without formal court proceeding, 3,914 (25 per cent) with proceedings but without trial and 56 (0.3 per cent) at trial.
Failure to recruit and retain staff and invest in life-saving drugs or equipment harms patient care.
In the first 70 years of the NHS, the average annual budget rise was 3.7 per cent. However, between 2009/10 and 2018/19, the average funding growth each year was just 1.5 per cent.
In 2020, the Institute for Public Policy Research estimated that since 2014 public health grants have been cut by around £13.20 per person in England.
The poorest parts of England have seen the deepest cuts to their public health budgets, worsening long-standing health inequalities between the north and the south.
Britain has markedly fewer doctors and nurses than similar countries relative to the size of its population and fewer CT scanners and MRI machines.
Britain performs less well than similar countries on the overall rate at which people die when successful medical care could have saved their lives.
According to the Institute for Fiscal Studies, the mortality rate in Britain among people treated for some of the biggest causes of death, including cancer, heart attacks and stroke, is higher than average among comparable countries.
Britain also has high rates of child mortality around birth and comes sixth-lowest out of the richest G7 countries in health spending.
In March 2019, a British Medical Association report highlighted the deterioration of public health services and called for the cuts to the NHS budget to be stopped.
In June 2019, the Health Foundation and the King’s Fund issued a joint statement, urging the government to “make a clear and urgent commitment to restoring £1bn of real-terms per head cuts to the public health grant.”
The two organisations said that cuts to the public health grant made since 2015/16 are having a major impact on local services.
They said: “Failing to act now would be a false economy, placing further pressure on the NHS and wider public services.”
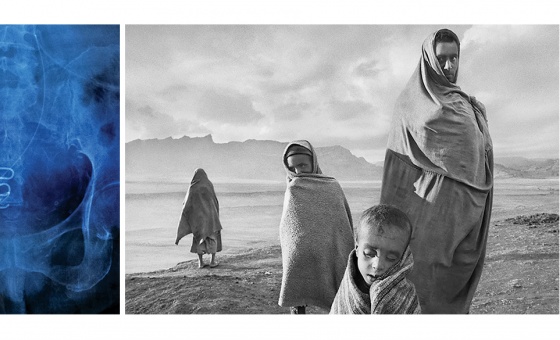
The NHS Resolutions report also reveals that maternity services account for 54 per cent of claims, underlying the appalling record of the Tories in failing to meet the needs of women, especially those from black and ethnic minority backgrounds who feature disproportionately in clinical errors.
NHS Resolution is anticipating a huge increase in claims related to the Tories’ mishandling and criminal negligence throughout the pandemic, in particular from the families of 20,000 care home residents sent into care homes from hospitals with Covid-19 infections.
The Royal College of Nursing (RCN) has condemned the government’s continued lack of investment in health and social care services and staff following the March 2021 Budget announcement.
RCN chief executive and general secretary Dame Donna Kinnair said: “This Budget was intended to show the path to recovery — but nursing staff won’t have seen one today.
“Their own recovery feels a long way down the government’s list of priorities.
“Nursing staff need rest and recuperation and for ministers to fund ongoing access to confidential counselling, bereavement and psychological trauma support.
“Long Covid must be recognised as an occupational disease, with more specialist clinics to meet demand.
“The government must get staffing levels back to pre-Covid levels as a minimum, particularly in areas like intensive care where ratios have been diluted to unsafe levels.”