This is the last article you can read this month
You can read more article this month
You can read more articles this month
Sorry your limit is up for this month
Reset on:
Please help support the Morning Star by subscribing here
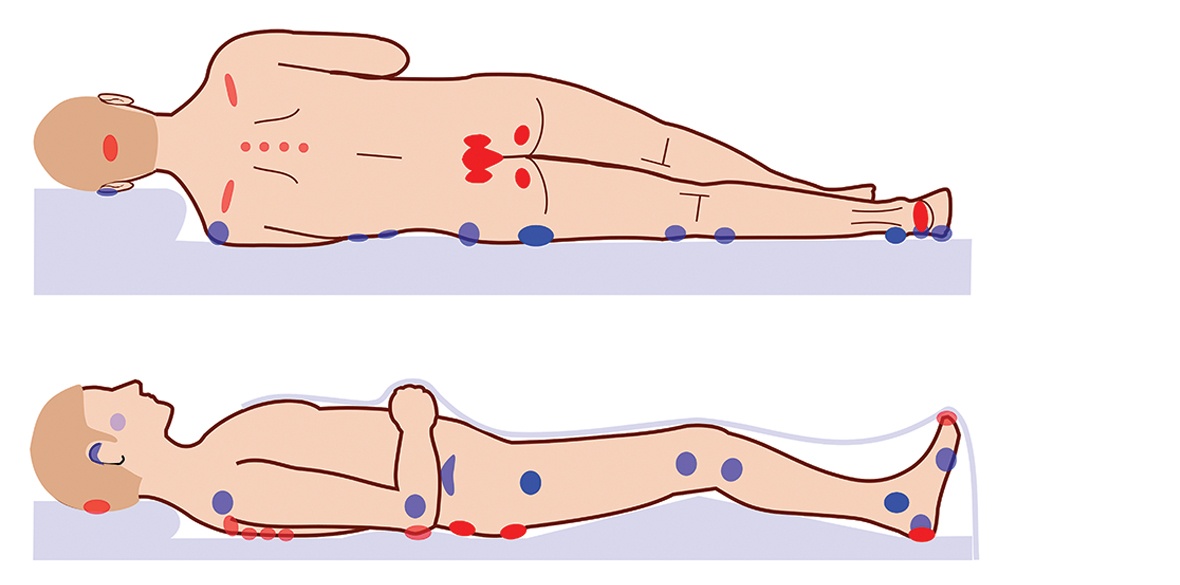
THIS WEEK, on Thursday November 17, an awareness campaign called Stop the Pressure Day was launched by the Spinal Injuries Association (SIA) in order to share advice and campaign for better understanding regarding the devastating physical, mental and financial costs of pressure sores.
The SIA claims failings in specialist knowledge about spinal cord injury in the healthcare sector are preventing early detection of pressure ulcers and this lack of awareness is leading to dangerous and life-threatening consequences such as sepsis, costing lives and the NHS millions.
Sue Mould was injured in January 2015 when she was out jogging and a falling tree branch hit her on the head, leaving her paraplegic and with chronic neuropathic pain.
Following years of rehabilitation, Sue was finally getting her life back on track when in 2021 she noticed a small blister developing on her ankle that didn’t heal. She went to her GP surgery where her wound was dressed by the nurse.
“Every single time I went there I explained it’s really worrying me; I am getting quite scared by it now as it is not healing and seems to be getting worse and I won’t know what is going on because I am paraplegic. The nurse would scratch her head and say yes it should have healed by now and I can’t understand why it hasn’t.”
According to Sue, month after month they were happy to just keep changing the dressing on her ankle without any simple things like a blood test being conducted.
“I told them time and time again that I wouldn’t be able to recognise if anything more sinister was going on as I can’t feel pain in that area. I also repeatedly asked to be referred and for a tissue viability nurse to take a look. I’m told they did look at a photo and made their judgements based on this. I am convinced if I had been able to see a GP, things would have been different.”
Sue asked so many times for a referral and was refused, until she asked to undertake a complaint. It was only at that point the GP contacted her on the phone to say it may need to be referred.
“It just felt like a constant stream of incompetence, a complete lack of knowledge and understanding of the issues surrounding my skin as a paraplegic. They seemed woefully inadequate in accepting you can’t feel pain like others, and they need to factor that in to investigating what is going on.”
It wasn’t until a routine check at her spinal unit that Sue was told she needed to go straight to her nearest hospital.
When she arrived at A&E, they undertook blood tests and found Sue’s infection markers were around 200, whereas normal is about nine or 10. The doctor told her she wouldn’t have lasted another 24 hours.
During the following five months in hospital, Sue had at least 20 visits to theatre as they had to open the wound and clean it every week and check for new infection.
Sue said: “When the surgeon arrived, he said he expected to see me doubled up on the bed in agony, but because I am paraplegic, I wasn’t feeling the pains that other people feel. I just felt sick. This is why pressure ulcers often don’t get picked up on because without blood tests or an MRI they can’t really tell when something is serious.”
Sue contacted the SIA as soon as she was admitted, and Karen Biggs, a specialist nurse in spinal cord injury, who had supported her previously, sent an emergency care plan to the hospital the next day.
The plan explained to nursing staff the specialist care that Sue should receive to prevent further issues arising. According to Sue the problem was they didn’t always read it due to the high turnover of staff.
She accepts the treatment she had in hospital saved her life, but her issues lay with her care because she believes the hospital didn’t seem to have any awareness of how to deal with someone who was paraplegic and at times that was very distressing.
“Coming back from theatre and being told to use bed pans I was made to feel awkward because I can’t use a bed pan as I am paraplegic!”
“I have never been through anything so distressing as having to be in hospital for so long, having to go down to theatre every single week. I know it is hard for nurses, but I was really struggling with my mental health as a consequence of everything that was going on.”
Sue eventually went home at the end of January this year after five months in hospital.
“When I got home, I have never felt so alone and so low and I have had to cope with a lot in my life since my accident. You start thinking is this my life now, will I have to just think about the next medical incident that is going to land me back in hospital? I also didn’t realise the impact all this had on my family.
“When I think that it all could have been avoided, I felt lost, I felt so sad, distressed and angry — so many emotions.”
At the last count, the treatment of pressure ulcers was costing the NHS £3.8 million a day and more than £20m a year in litigation in 2018, according to the Nursing Times. In a recent survey by Spinal Injuries Association, 75 per cent of those who took part said they had had up to five pressure ulcers.
Biggs believes emergency care plans are vital and should be always attached to your records, but according to the SIA this is not automatic, and the patient needs to consult with the hospital to have it added. “Knowledge is power, and we support many to become an expert in their own condition,” she said.
“We know that it is not always easy or possible to spot an ulcer in a hidden area and we support education among community nurses, general hospitals, and the care sector. Simple specialist knowledge can save lives and mental trauma.”
Nik Hartley OBE, CEO of the SIA, said: “We must have a health and care system that works for everyone — including spinal cord-injured people. At SIA we are committed to making sure we are training up healthcare professionals in every region of the country to equip them to care for spinal-cord injured people, while continuing to provide specialist services to spinal cord-injured people support the work of the NHS.”
More informatuion is available at www.spinal.co.uk.
Ruth F Hunt is an author and freelance journalist.